Abstract
Introduction: NHL is a heterogeneous disease which frequently occurs in older adults. Patients (pts) with NHL have an increased risk of non-NHL malignancies (NNM; Morton, JCO, 2010) and published guidelines emphasize the importance of standard of care cancer screening in this population (Hallek, Blood, 2018). Comorbidities are associated with a more aggressive clinical course and shorter survival in pts with NHL. We hypothesized that comorbidities, measured using the three-factor risk estimate scale (TRES; Gordon, CCR, 2021), would be associated with increased risk of death due to NNM. These findings could have important implications for cancer screening in comorbid pts with NHL.
Methods: We included pts in SEER-Medicare with NHL (ICD-O-3/WHO recodes 25012, 33041 and 33042) diagnosed between 2008-2017. Medicare claims were available through 2019. All cases had a pathologically confirmed diagnosis of NHL, age at cancer diagnosis >65 years and continuous coverage in Medicare parts A, B and D with no HMO coverage for the 12 months preceding diagnosis and for 12 months, or death if sooner, after diagnosis. Pts were excluded who were diagnosed on death certificate or at autopsy. Other cancers were identified in SEER. Comorbidities were assessed using the TRES comorbidity score, previously known as CLL-CI (Gordon, CCR, 2021). This index evaluates endocrine, vascular and upper gastrointestinal organ systems, assigning pts to low, intermediate and high-risk groups based on overall survival. Chi-square or t-test was used to compare pt characteristic distributions. Kaplan-Meier estimate and multivariable Cox regression with competing risk were used to test the association between NNM and TRES score.
Results: Our cohort consisted of 40,486 pts with NHL. Median age was 77 years, 49.5% were female, 91% were white, 3.3% Hispanic and 2.5% black. 51% were unmarried. 62% received treatment for NHL during the study period, the most common type of treatment was chemoimmunotherapy (31%). TRES score was low in 41%, intermediate in 37% and high in 22%. 23.6% had a cancer diagnosis prior to NHL and 10.4% after. The most common types of cancer preceding NHL diagnosis were prostate (29%), breast (16%), melanoma (9%), colorectum (6%), bladder (6%) and lung (5%). The most common cancer types after NHL diagnosis were colorectal (16%), head and neck (11%), lung (7%), bladder (5%), MDS/AML (5%) and melanoma (5%).
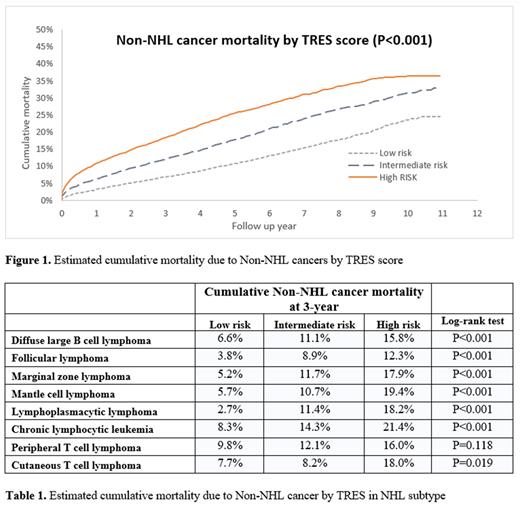
Cause of death was reported and analyzed in 30,155 pts which were included in the primary analysis of NNM specific survival. After a median follow up of 33 months, a total of 14,473 deaths occurred, 48% of all subjects in whom cause of death was reported. The most common cause of death was NHL (49%, N=7,110) followed by NNM in 36% (N=5,183) and other causes in 15% (N=2,180). Compared to pts with a low TRES score, intermediate and high-risk scores were associated with an increase in NNM (p<0.001, Figure 1). In multivariable models, hazard ratios (HR) were 1.41 (95%CI 1.32-1.51) for intermediate and 1.94 (95%CI 1.80-2.08) in high risk pts. Other variables associated with non-NHL cancer mortality were NHL subtype, stage, age, gender, marital status and initial treatment type.
The most common NHL subtypes were chronic lymphocytic leukemia (CLL N=8,368), diffuse large B cell lymphoma (DLBCL, N=8,292), follicular lymphoma (FL, N=3,870), marginal zone lymphoma (MZL, N=2,597), mantle cell lymphoma (MCL, N=1,208), peripheral T cell lymphoma (PTCL, N=851), cutaneous T cell lymphoma (N=773) and lymphoplasmacytic lymphoma (LPL, N=495). TRES score was associated with NNM in all NHL subtypes, except for PTCL (Table 1). In pts who died, the percent due to NNM by NHL subtype was 50% in CLL, 25% in DLBCL, 40% in FL, 50% in MZL, 18% in MCL, 21% in PTCL, 39% in CTCL and 74% in LPL. The most frequently cited causes of death from NNM were MDS/AML, colorectal, lung and head and neck cancers.
Discussion: Other cancers are a common cause of death in older adults with NHL, particularly in pts with indolent B cell subtypes (range, 40%-74%), and comorbidities further increase the risk of death from NNM. This may be due to the combinatorial effects of NHL and comorbidity on immunologic and metabolic regulation. These results have important implications for the treatment of older adults with NHL and highlight the need for close monitoring and the development of adapted cancer screening guidelines in this population.
Disclosures
Nastoupil:ADC Therapeutics, BMS, Caribou Biosciences, Epizyme, Genentech/Roche, Gilead/Kite, Genmab, Janssen, MEI, Morphosys, Novartis, Takeda: Honoraria; Genentech/Roche, MEI, Takeda: Other: DSMC; BMS, Caribou Biosciences, Epizyme, Genentech, Gilead/Kite, Genmab, Janssen, IGM Biosciences, Novartis, Takeda: Research Funding. Ferrajoli:Beigene: Research Funding; AstraZeneca: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees. Danilov:Beigene: Consultancy; Astra Zeneca: Consultancy, Research Funding; Takeda Oncology: Research Funding; Morphosys: Consultancy; Bayer Oncology: Research Funding; MEI: Consultancy, Research Funding; Cyclacel: Research Funding; Bristol-Meyers-Squibb: Consultancy, Research Funding; Pharmacyclics: Consultancy; Abbvie: Consultancy, Research Funding; Nurix: Consultancy, Research Funding; Genentech: Consultancy; Incyte: Consultancy; GSK: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal